Borderline personality disorder (BPD) features a fragile self-image that often results in impulsive behaviors and volatile emotional states. This condition lies on the border between psychotic disorders, which cause a disconnection from reality, and neurotic disorders, characterized by severe emotional distress. Hooked on Hope Mental Health acknowledges the heightened risk individuals with BPD face regarding substance misuse and other mental health issues. Our outpatient mental health treatment program in Atlanta is designed to assist clients in identifying their challenges and securing the right mental health care.
What Is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder (BPD) is a profound mental health condition impacting a person’s self-perception and their interpersonal relationships. It typically manifests in early adulthood and can significantly interfere with an individual’s life. However, with professional intervention, many see substantial improvements.
BPD may develop due to a combination of genetic factors, brain serotonin imbalances, or early trauma. It’s present in approximately 1.6% of the general population, with rates climbing to 20% among psychiatric inpatients. Characteristics of BPD include intense mood swings, changing interests, an unstable self-image, and engagement in harmful activities like substance use or self-harm. Effective management of BPD requires specialized, professional treatment.
Types Of BPD
Borderline Personality Disorder presents in various forms, with individuals exhibiting different symptom clusters.
Mental health experts have classified four primary subtypes of BPD:
- Discouraged BPD: Dominated by feelings of inadequacy, emotional dependency, and a profound fear of rejection.
- Impulsive BPD: Identified by emotional volatility, impulsive decisions, and engagement in risky behaviors.
- Petulant BPD: Characterized by unpredictable moods, quick temper, and intense fear of being abandoned.
- Self-Destructive BPD: Marked by self-harming actions, self-defeating behaviors, and a persistent sense of emptiness.
At Hooked on Hope Mental Health, our compassionate team specializes in addressing these varied expressions of BPD, ensuring tailored and effective support for every individual. Call us 24 hours a day at 470-287-1927 or via our online contact form to speak with an admissions coordinator about the best BPD treatment options for your situation.
Diagnosing BPD: Assessment and Evaluation
At Hooked on Hope, our experienced mental health professionals begin with a thorough assessment to accurately diagnose Borderline Personality Disorder (BPD). This evaluation encompasses a complete review of the individual’s medical and psychiatric history, an in-depth analysis of their emotional health, and an assessment of how these symptoms impact their everyday life and relationships. Recognizing BPD is crucial for developing a personalized treatment strategy tailored to the specific challenges and needs of each individual. We are dedicated to providing compassionate, evidence-based care from the outset of the diagnostic process.
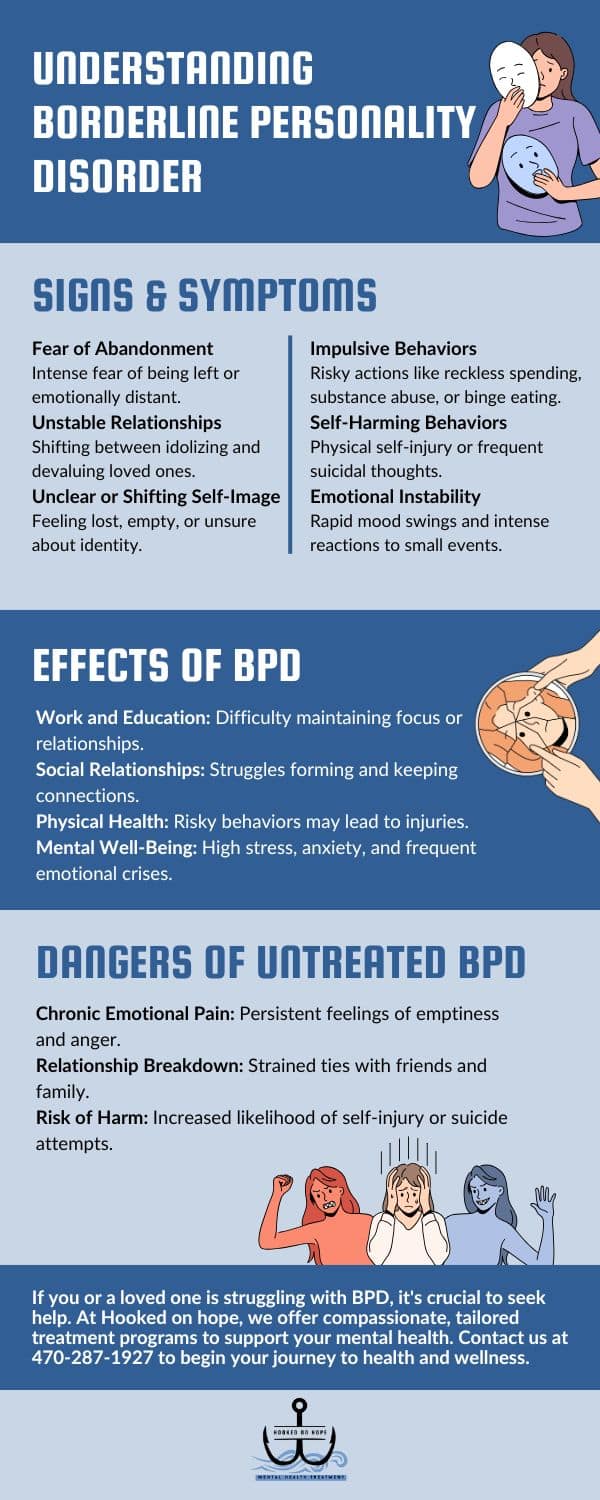
Signs Of Borderline Personality Disorder
The manifestations of Borderline Personality Disorder (BPD) can vary widely, and not all individuals will exhibit the same symptoms.
Commonly observed signs of BPD include:
- Emotional instability and challenges in managing intense emotions
- Persistent feelings of worthlessness
- A pattern of unstable and intense interpersonal relationships
- Rapid changes in views and feelings about others
- Chronic fear of abandonment
- Frequent self-harming behaviors or threats of self-injury
- Impulsivity and engagement in risky behaviors
- Proneness to intense anger or sudden mood swings
- A tendency to avoid responsibility for one’s actions
- Episodes of paranoia or dissociation from reality
- Frequent suicidal thoughts or behaviors
- Extreme and swift shifts in self-identity, mood, and perception
- Difficulties with trust and maintaining stable relationships
It is important to note that not everyone with BPD will experience all these symptoms, but many will encounter several throughout their lives. Symptoms often begin in adolescence or early adulthood, although signs can sometimes manifest in later childhood.
BPD frequently co-occurs with other mental health conditions such as depression, anxiety, or substance abuse, complicating the diagnosis. Transparent communication of all symptoms and concerns is crucial during a psychiatric evaluation to ensure a precise diagnosis and an effective treatment plan. If you or a loved one is struggling with BPD, our outpatient treatment program in Atlanta is ready to assist. Contact us 24 hours a day at 470-287-1927 or via our online contact form.
Risk Factors for Borderline Personality Disorder
Studies reveal that Borderline Personality Disorder (BPD) generally arises from a combination of genetic, environmental, and social factors.
These elements can significantly impact the risk of developing BPD:
- Genetic Factors: There’s a familial trend with BPD, indicating that genetics may contribute to its development.
- Brain Structure and Function: Individuals with BPD often exhibit changes in brain areas responsible for impulse control and emotion regulation.
- Childhood Trauma: Many people with BPD have experienced early trauma, such as abuse or neglect, which critically impacts their emotional development.
- Early Relationship Turmoil: Having unstable or conflict-ridden relationships during formative years can trigger or exacerbate BPD symptoms.
These factors don’t necessarily cause BPD but increase the susceptibility to developing the disorder. Understanding these risk factors is crucial for preventing BPD and devising effective treatments for those affected.
Difference Between Borderline Personality Disorder and Bipolar Disorder
Borderline Personality Disorder (BPD) and bipolar disorder are frequently confused due to their overlapping symptom of mood instability; however, they are distinctly different conditions. BPD is marked by rapid mood shifts often triggered by external stresses or social interactions, leading to intense, unpredictable emotional responses. These shifts are typically driven by fears of abandonment or rejection, potentially resulting in impulsive behaviors.
In contrast, bipolar disorder is characterized by more extended mood episodes that can last for days or weeks and are less influenced by immediate external factors. These mood swings range from mania—periods of excessive energy and euphoria—to depressive episodes, characterized by profound sadness and lethargy.
Understanding the distinctions between these conditions is vital for accurate diagnosis and treatment. Bipolar disorder involves significant changes in sleep, cognition, and activity levels, which are not as prevalent in BPD. In BPD, emotional reactions are more about immediate circumstances, closely tied to self-image and interpersonal relationships.
Can Borderline Personality Disorder Be Prevented?
Borderline Personality Disorder stems from a complex mix of genetic, neurological, and environmental influences, which makes prevention challenging. Nevertheless, recognizing early signs can substantially alter the disorder’s trajectory. A familial predisposition to BPD underscores the importance of being vigilant for early symptoms.
Routine mental health assessments can identify potential early indicators of BPD before more severe symptoms appear, allowing for earlier and possibly more effective interventions. Establishing strong support systems, enhancing access to counseling services, and fostering open dialogues about mental health are crucial steps toward mitigating BPD’s severity.
While it may not be possible to completely prevent BPD, early detection and intervention can profoundly lighten the burden for those affected. Staying informed about BPD and maintaining communication with healthcare professionals are vital for securing optimal treatment and support.

How is BPD Treated?
Outpatient therapy for Borderline Personality Disorder (BPD) employs a mix of techniques, prominently featuring Dialectical Behavioral Therapy (DBT). As a refined form of Cognitive Behavioral Therapy (CBT), DBT is valuable not only for BPD but also for other mental health conditions.
DBT aids patients in managing their emotions and reactions, providing strategies to transform detrimental behavioral patterns. Through one-on-one sessions, individuals delve into the roots of their volatile emotions and actions, learning to cultivate balanced and constructive responses. This method progressively strengthens resilience, effective coping mechanisms, and a positive self-image, which in turn improves interpersonal relationships.
Advances in BPD treatment now offer significant improvements in life quality for individuals with BPD, highlighting the effectiveness of modern therapies.
Commitment is essential in the therapeutic process, which may include individual therapy, medications, or a combination of both, based on the individual’s needs. In cases of acute distress, a brief hospitalization might be necessary to stabilize the individual and develop a comprehensive treatment plan.
It is also important to note that BPD often coexists with other mental health disorders such as mood disorders, anxiety disorders, substance abuse disorders, eating disorders, ADHD, bipolar disorder, and somatoform disorders. Recognizing these co-occurring conditions is crucial in delivering an all-encompassing and effective treatment.
The Impact of Untreated Borderline Personality Disorder
Addressing Borderline Personality Disorder (BPD) promptly with professional intervention is crucial. Without treatment, BPD can cause profound distress not only to the individual but also to those around them, often leading to unstable relationships with family, friends, and coworkers. The emotional instability characteristic of BPD can hinder a person’s ability to function effectively in educational or professional environments, exacerbating the disorder’s detrimental effects.
Individuals with untreated BPD are more likely to engage in high-risk behaviors, such as reckless driving or unsafe sex, heightening their risk of accidents, unwanted pregnancies, or encounters with violence. A particularly alarming aspect of BPD is the propensity for self-harm, posing significant risks of lasting physical and psychological damage. Additionally, the likelihood of suicide increases dramatically in those with untreated BPD, making early and consistent therapeutic support essential.
BPD Treatment Options
Psychotherapy remains central to treating Borderline Personality Disorder, crucial for helping individuals reclaim control of their lives and foster healthier relationships. Psychotherapy aims to help individuals understand the underlying factors influencing their thoughts, emotions, and behaviors, thereby developing healthier cognitive and interactional patterns.
Highlighted psychotherapy interventions for BPD include:
- Dialectical Behavioral Therapy (DBT): DBT is considered highly effective for BPD treatment. It focuses on mindfulness, emotional regulation, interpersonal effectiveness, and distress tolerance, equipping individuals with tools to manage intense emotions and minimize harmful behaviors.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals examine their thought processes and emotional responses, aiming to replace negative patterns with positive ones. It’s particularly useful for addressing impulsivity and unstable emotions associated with BPD.
- Group Therapy: Provides a supportive environment where individuals can share experiences and coping strategies under professional guidance, enhancing self-expression and social skills.
- Individual Therapy: Offers a tailored approach to therapy, allowing deeper exploration of personal issues with a therapist in a confidential setting.
- Family Therapy: Involves family members to improve communication and understanding within the family, essential for supporting the individual with BPD.
- Holistic Therapy: Practices like music, meditation, and art therapy complement traditional treatments by promoting overall well-being and emotional balance.
- Medication-Assisted Treatment: While not the primary treatment for BPD, medications may be used to manage specific symptoms like mood swings or anxiety, facilitating more effective engagement in psychotherapy.

Comprehensive Approach to Healing with BPD Treatment
BPD treatment is highly personalized, combining various psychotherapeutic interventions and support services to foster long-term emotional health. At Hooked on Hope Mental Health, our team is committed to providing customized care that addresses the unique challenges faced by each individual with BPD. We strive to create a supportive and understanding environment that encourages positive change and personal growth.
If you or a loved one is dealing with Borderline Personality Disorder in Atlanta, GA, reach out to us at Hooked on Hope Mental Health. Our experts are here to support you through a tailored treatment plan that fosters recovery and well-being. Contact us at 470-287-1927 or via our online contact form for more information on our specialized BPD treatment services.
Borderline Personality Disorder Treatment in Atlanta, GA
Dealing with borderline personality disorder is challenging, but you are not alone. Hooked on Hope Mental Health in Atlanta, GA, offers specialized outpatient treatment for Borderline Personality Disorder within a supportive and nurturing environment. Our experienced team is well-versed in the complexities of BPD and tailors therapy to meet individual needs, aiming to empower clients to manage their mental health with strength and resilience.
Interested in learning how we can assist in your path to wellness? Contact us at 470-287-1927 or via our online contact form. Our compassionate staff is eager to introduce you to our program, answer your queries, and support you every step of the way.